PURA 101
What is PURA Syndrome?
PURA Syndrome is a rare genetic disorder that affects neurodevelopment. It was first described in medical literature in October of 2014. PURA syndrome arises when there is a genetic alteration affecting one of a person’s two copies of the PURA gene. The defect can be a single letter spelling change within the gene, a small insertion or deletion within the gene, or even a larger deletion removing one whole copy of the gene (and potentially many neighbouring genes as well).
- Where is the PURA gene located? On the long arm of chromosome 5 (at position 5q31.3)
- What does the PURA gene do? It encodes for a protein, pur-alpha, which is expressed in all tissues, including the brain, muscle, heart, and blood.
- pur-alpha has an important role in the normal development of the brain
- The pur-alpha protein’s role in the human cell includes:
- regulatory functions in DNA replication
- transcription and translation of mRNA
What is the Life Expectancy for someone with PURA Syndrome?
PURA syndrome is a neurodevelopmental disorder, not a degenerative disorder. Survival into adulthood is expected, barring illness or complications.
Of those we know of diagnosed with PURA since 2014, there are many individuals in their 20’s, 30s, 40s and even one in their 50’s living with this syndrome. As more people are diagnosed and complete the Global Patient Registry, more information about the natural history of the syndrome will become available.
Prevalence
To date, the PURA Syndrome Foundation is aware of about 750 individuals with PURA Syndrome worldwide. However, given that modern genomic tests are becoming cheaper and more widely accessible, it is likely that hundreds more people will be diagnosed with PURA syndrome in the next few years.
Physical Features
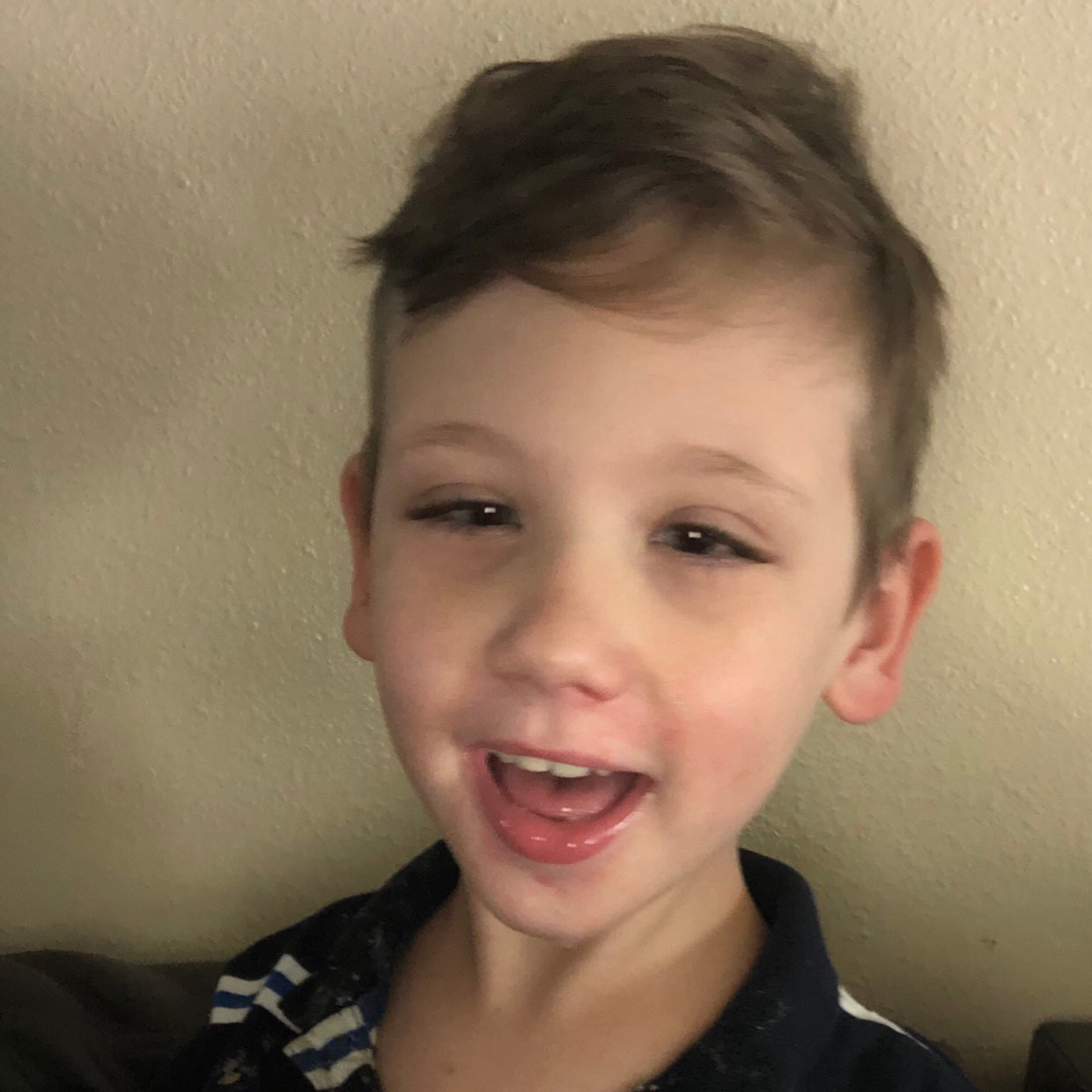
Individuals with PURA syndrome can be affected in different ways, but common physical features include:
- Low muscle tone (Hypotonia)
- Flexible joints – particularly fingers, wrists and elbows
- Full cheeks
- Open lips in resting position
- Soft skin and/or sensitive skin
- High arched palate
- High anterior hairline
- Almond shaped eye openings
- Growth: Birth weight is usually in the normal range, and affected children tend to grow appropriately.
- Puberty: can be early-onset (‘precocious’) or delayed.
Behavioral Characteristics
Various behavioural traits have been observed in individuals with PURA syndrome, and these tend to correlate with the overall degree of developmental delay.
- Loving and very social
- Sensory processing challenges (sensitive to certain textures, loud noises, empathetic to other children crying)
- Hand-flapping, hand-biting, hand sucking
- Anxiety
- Some have increased aggression and can self harm
- Sleep disorders
Cognitive Abilities
All children with PURA syndrome who have been identified to date have at least a moderate to severe degree of learning disability and developmental delay.
- Speech Language Delay
- Most individuals with PURA syndrome remain nonverbal. Some affected individuals are able to use single words, short phrases or simple sentences.
- It is generally recognized that affected individuals have better receptive language skills (understanding of spoken language) than expressive language skills. Therefore, many parents choose to explore various Augmentative and Alternative Communication (AAC) aids as a means of enhancing and enabling expressive communication. This may range from simple options such as signing and gesturing through to symbol-based systems, and the latter may entail the use of touch-screen devices or even eye-gaze technology in some cases.
- Learning
- All individuals that we know of have moderate to profound learning disability and require specialist support with learning.
- Gross and Fine Motor delay
- Late or no crawling, late walking or limited to no mobility
Medical Issues
- Hypotonia (Low muscle tone)
- Seizures and seizure-like abnormal movements
- Feeding difficulties
- Respiratory problems (including obstructive and central apneas)
- Hypersomnolence (excessive sleepiness)
- Constipation
- Abnormal vision
- Temperature instability
- Excessive hiccups
- Orthopedic issues including hip dysplasia and scoliosis
- Endocrine disorders such as Vitamin D deficiency
- Exaggerated startle response
Disposition
Individuals with PURA syndrome tend to be very social and friendly people.
Genetics/Inheritance
In most affected individuals, the genetic alteration causing PURA syndrome will have arisen as a new change (i.e. it was not inherited from either parent). However, rarely it can be inherited from a parent who carries the genetic alteration in some, but not all, cells of their body.
- Can it happen again? If neither parent is found to carry the same genetic alteration in PURA when testing is performed on DNA extracted from their blood, there is a very low chance of having another child with the same genetic alteration. Empirically, this chance is less than 1%. This residual risk is due to a phenomenon known as ‘gonadal mosaicism’, in which a parent may have a cluster of cells within their reproductive organs that carries the genetic alteration in PURA (but this cannot be detected on a blood test and there is currently no effective way to test for gonadal mosaicism).
Testing & Diagnosis
Diagnosis is usually made using a ‘next generation sequencing technology’, such as whole exome sequencing or whole genome sequencing, Sometimes a ‘gene panel’ test will be performed, focusing on genes linked to neurodevelopmental disorders or genetic epilepsies. These are all very broad types of genetic test that are suitable for diagnosing PURA syndrome, which cannot confidently be diagnosed by clinical assessment alone.
- Synonyms of PURA syndrome
- PURA-Related Neurodevelopmental Disorder
- Intellectual Developmental Delay, autosomal dominant 31
- Differential diagnosis – Disorders with similar characteristics are:
- Central Hypoventilation syndrome [OMIM209880]
- Spinal Muscular Atrophy [OMIM253300])
- Myotonic Dystrophy [OMIM160900]
- Prader Willi syndrome [OMIM176270]
- Angelman syndrome [OMIM105830]
- Rett syndrome [OMIM312750]
- Pitt-Hopkins syndrome (OMIM610954)
- Metabolic conditions / disorders
What is 5q31.3 deletion syndrome and how does it differ to PURA Syndrome?
The 5q31.3 deletion syndrome is very similar to PURA syndrome, but it is not exactly the same. Whereas individuals with PURA syndrome have a genetic alteration that solely affects one of their two copies of the PURA gene, individuals with the 5q31.3 deletion syndrome are lacking a segment of DNA from one of their two copies of chromosome 5 (within the ‘5q31.3 cytogenetic band’). Usually, a 5q31.3 deletion affects not only one copy of the PURA gene but also some of the adjacent genetic code.
The chromosomal deletions causing the 5q31.3 deletion syndrome can vary significantly between affected individuals. Sometimes they can be small. Sometimes they can be very large, including dozens or even hundreds of other genes. No two individuals with the 5q31.3 chromosomal deletion syndrome have been found to have exactly the same deletion.
Importantly, any chromosomal deletion affecting the PURA gene will cause PURA syndrome (irrespective of how many neighboring genes it may also affect).. This means that individuals with the 5q31.3 deletion syndrome do have PURA syndrome, but we recognize that individuals with the 5q31.3 deletion syndrome tend to be more severely affected. It is most likely that some of the other genes included in an individual’s deletion may be contributing to the severity of their clinical presentation. There are a number of nearby genes that may be important in this respect.
The 5q31.3 deletion syndrome is much rarer than PURA syndrome.
Management Recommendations
The treatments for PURA syndrome are directed toward the specific symptoms that are apparent in each individual. Treatment will require the coordinated efforts of a multidisciplinary team, ideally with the involvement of a neurologist, geneticist, pediatrician, respiratory physician, ophthalmologist and orthopedic surgeon.
Epilepsy, present in over half of the PURA syndrome cases, can be very difficult to manage effectively. While some individuals have responded well to specific anti-epileptic drugs, refractory (drug resistant) seizures are common. Therefore, further research into seizure causes and management is required.
There are currently no evidence-based consensus management guidelines for PURA syndrome. However, it is recommended that consideration be given to the following
- At diagnosis
- A formal developmental assessment, if not already completed
- EEG (measurement of brain’s electrical activity), if seizures are suspected
- Brain imaging with MRI, especially in those with confirmed or suspected seizures, apnoeas or visual problems
- A formal assessment of the eyes, which may include ‘electrodiagnostic’ tests of vision
- Respiratory studies, including sleep study, especially if there are concerns about possible apnoeas
- Feeding assessment, including a formal assessment of swallowing (to make sure that it is safe and there is no risk of aspiration) and an assessment for constipation
- Baseline ultrasound scans of heart and kidneys to exclude any congenital malformations (but note that these appear to be uncommon in PURA syndrome)
- Musculoskeletal assessment for evidence of hip dysplasia or scoliosis
- Vitamin D measurement
- Bone density assessment, especially in older children and adults who are nonambulatory and taking long-term antiepileptic drugs, and any affected individual with a history of a low energy (‘pathological’) fracture
- After diagnosis
- Regular follow up with a developmental pediatrician
- EEG (measurement of brain’s electrical activity), in the event of suspected seizures
- Ongoing monitoring for any evidence of swallowing problems or constipation
- At least annual assessment for hip dysplasia and scoliosis
- Speech and language support
- Physiotherapy and occupational therapy, as required
- Regular eyesight checks
See also: Tables 2, 3 and 4 in the PURA-Related Neurodevelopmental Disorders